Understanding Restrictive Practices in Australian Health care & Aged Care
A Complete Guide for Nurses to Promote Safety, Dignity, and Compliance
🔍 What Are Restrictive Practices?
Restrictive practices refer to any action or intervention that restricts a person's movement, decision-making, or freedom — often used to manage behaviours of concern in healthcare or aged care settings. While sometimes necessary for safety, these measures carry serious ethical and clinical implications.
In Australia, the Aged Care Act 1997, Quality of Care Principles 2014, and the NSQHS Standards outline strict criteria to ensure restrictive practices are used only:
As a last resort
In the least restrictive form
For the shortest possible time
With informed consent and appropriate documentation
Why Nurses Must Understand This
As an RN or EN in Australia, you're accountable for ensuring care aligns with Standard 1 (Clinical Governance) and Standard 2 (Partnering with Consumers) under the NSQHS. Misuse of restrictive practices can lead to:
Psychological harm to the patient
Regulatory non-compliance
Risk to your professional registration
The 5 Types of Restrictive Practices Explained
1. 💊 Chemical Restraint
Definition: The use of medication to control behaviour, not to treat a diagnosed condition.
Examples:
Sedating a patient with dementia to prevent wandering
Administering antipsychotics for aggression without a mental health diagnosis
Risks:
Falls, confusion, reduced quality of life
Breach of informed consent
Alternatives:
Music therapy, pain assessment, validation therapy
Engage the patient in calming, structured routines
2. 🤲 Physical Restraint
Definition: Any physical hold or action to subdue or limit a person’s movement.
Examples:
Holding a patient to prevent them from pulling out an IV
Manually guiding someone back to their room against resistance
Risks:
Bruising, fractures, loss of trust
Potential breach of human rights
Alternatives:
De-escalation, therapeutic communication, and redirection strategies
3. 🔒 Mechanical Restraint
Definition: Use of devices to restrict movement, not for therapeutic purposes.
Examples:
Bed rails, lap belts, tray tables fixed to chairs
Risks:
Pressure injuries, immobility, feelings of imprisonment
Alternatives:
Sensor mats, posture-supporting seating, staff supervision
4. 🚪 Environmental Restraint
Definition: Restricting a person's access to parts of their environment.
Examples:
Locking exits to prevent wandering
Removing mobility aids or closing doors to communal spaces
Risks:
Isolation, anxiety, reduced quality of life
Alternatives:
Safe walking paths, supervised access, coded but unlockable doors
5. 🚷 Seclusion
Definition: Placing a person alone in a room or space where they cannot freely leave.
Examples:
Locking someone in a quiet room due to aggression
Isolation during a behavioural episode
Risks:
Trauma, emotional harm, regression in behaviour
Alternatives:
Calming environments, 1:1 supervision, sensory modulation
📉 The Impact of Overuse
Restrictive practices can cause:
Emotional distress and trauma
Functional decline and dependency
Violations of a person's autonomy and rights
Legal and professional risk for providers and clinicians
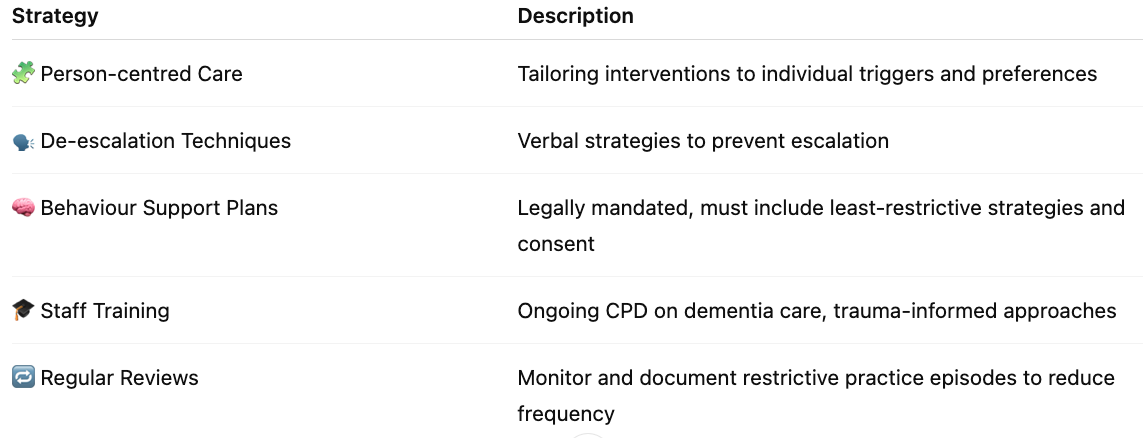
✅ Evidence-Based Strategies to Reduce Use
⚖️ Legal Compliance for Nurses
Always document in the care plan and progress notes
Ensure informed consent or legal authorisation is obtained
Regularly review BSPs and update based on behavioural trends
Use alternative strategies first and record attempts
Align practice with:
Aged Care Quality Standards
🧭 Final Thoughts: Your Role as a Nurse
Think of restrictive practices like an emergency brake: useful only when all other systems fail. As a nurse, your power lies in prevention — creating therapeutic environments, building rapport, and leading the shift toward restraint-free care.